Supplementation is the provision of any food or drink other than breastmilk
received from the breast. Despite recommendations to the contrary,
non-medically indicated supplementation is common.17 Healthcare
professionals may recommend supplementation when it is not medically
indicated as a means of protecting parents from fatigue or distress. 17 New parents, particularly those with low breastfeeding
confidence, are vulnerable to advice suggesting breastfed infants be
supplemented with glucose water or infant formula.17
Providing formula or other liquids to breastfed infants when not medically
required may result in breastfeeding challenges including decreased breast
stimulation, milk production and maternal confidence, and increased risk of
delayed lactogenesis.18 Preventing unnecessary supplementation
of breastmilk substitutes is also important as exclusive breastfeeding to
six months protects the infant gut.19,20 Supplementation with
infant formula is also associated with lower breastfeeding duration rates. 21,22,23 When supplementation occurs, wherever possible, it
should be a short-term intervention with the goal to return the infant to
feeding at the breast.21
In Simcoe Muskoka:
- Approximately 30% (31.1% [29.8% - 90.7%])9 of babies are
fed infant formula in the first few days after birth, including:
- The prevalence of infant medical supplementation has more than
doubled in the last five years, from 2.8% (2.3% - 3.3%) in 2014 16 to 7.4% (6.7% - 8.2%) in 2019.9 The
reasons most commonly noted include “hypoglycemia”, “inadequate
weight gain” or “significant weight loss in the presence of
clinical indications”, and “other clinical indications”. 9
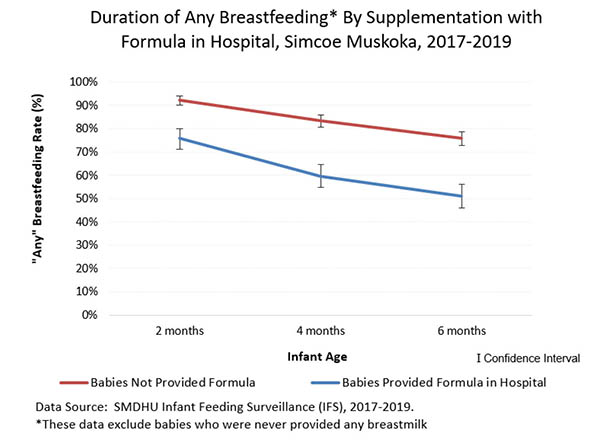
- Breastfed babies fed infant formula in hospital have lower rates of
breastfeeding at two, four and up to six months.12